June 2024 Provider News
Date: 06/28/24
In this issue:
- Apple Health Expansion - General, Benefits & Services, Billing, Payments, Provider Portal, HCA Resources
- General Updates - Updated Apple Health client forms: Medical Equipment and Supplies and Outpatient Rehabilitation, Self-Nomination Now Open For 2024 Immunize WA Awards, Occupational therapy for behavioral health conditions-Fact Sheet Feb 2024
- Quality - ADHD Follow Up on Kids, Telehealth, Antidepressant Medication Management (HEDIS Measure), Men’s Health Month
- Payment & Clinical Policy - July Policy Updates
- Pharmacy Update - Non-Contracted Drugs Update- Apple Health Expansion, Hyaluronic Acid Coverage Change Reminder
- Training/Education - Upcoming Provider Education Opportunities
______________________________________________________________________________________
Apple Health Expansion
What are the details of Open Enrollment for Apple Health Expansion?
Who is eligible?
- Washington residents age 19+, with income under 138% of the federal poverty level, who do not qualify for other Apple Health programs based on their immigration status, are not pregnant or did not have a pregnancy end in the last 12 months, and who are not eligible for qualified health plans with advance premium tax credits or federally funded medical assistance programs.
- Immigrants who have not met the five-year waiting period to become eligible for Apple Health are not eligible for Apple Health Expansion.
When does Open Enrollment start?
- Open Enrollment began on June 20, 2024, at 8:00 a.m.
How to apply?
Enrollment pathways for people ages 19-64:
- Online at www.wahealthplanfinder.org
- In-person through a Navigator
- Call 1-855-923-4633
Enrollment pathway for people ages 65+:
- Online at www.washingtonconnection.org
- In person at a DSHS CSO
What health plan options are there?
Enrollees may choose any Managed Care plan that offers Apple Health Expansion in their region. Coordinated Care is available statewide in all regions and offers Apple Health Expansion coverage. Service area map for Apple Health Expansion can be found here (PDF). If an enrollee does not select a Managed Care plan, HCA will auto-assign them to a Managed Care plan.
What happens if the program fills to capacity?
Once the Apple Health Expansion program is full (13,000 spots), denial letters will be sent from HBE to those who apply informing them the cap has been met. The letters will include other helpful information about programs they may be eligible for. At this time, there will not be a waitlist for Apple Health Expansion.
GENERAL
If an individual is already enrolled in a Qualified Health Plan (QHP), how will this population be transitioning to Apple Health Expansion?
- They will be automatically transferred with no actions needed if they meet all Apple Health Expansion eligibility criteria
What if the individual is already enrolled in an MCO that offers Apple Health Expansion?
- The HCA/HBE will automatically map the individual to the MCO affiliated with their QHP.
What if the member has an Ambetter PCP?
- Coordinated Care is taking steps to ensure PCP consistency and assign the member to the same PCP for their Apple Health Expansion coverage.
If the individual does not meet Apple Health Expansion eligibility criteria, there is no change; the individual stays with their QHP.
If an individual has a Washington Healthplanfinder account, but are NOT currently enrolled in a Qualified Health Plan (QHP,) what will they need to do?
- Log in to their account,
- Confirm their information is up to date, and
- Submit their application beginning at 8:00 a.m. on June 20, 2024.
If the member becomes incarcerated, are they termed from the Apple Health Expansion program?
- If a member is incarcerated, their eligibility for Apple Health Expansion will be suspended but not terminated.
What happens to the member’s coverage if they become documented?
- If an Apple Health Expansion member’s circumstances change, and they no longer meet the eligibility criteria for Apple Health Expansion, they should apply at Washington Healthplanfinder for other health care coverage options.
Will new or separate plan(s) be created to manage enrollees of the Apple Health Expansion program? If so, will there be a new name or how will members be identified on their ID Card?
- Apple Health Expansion members will have the same ID card as any other Apple Health member. Most benefits and services are the same. Providers will need to look in ProviderOne to confirm which coverage the member has, check the “Plan/PCCM name field.”
BENEFITS & SERVICES
Will Value-Added Benefits (VABs) offered by Coordinated Care be included for this program?
Coordinated Care will offer applicable Value-Added Benefits (VABs) and health incentives to Apple Health Expansion members, these include My Health Pays, Coordinated Care Harvest Bucks, and $100 towards adult eyeglasses or contacts. More information about My Health Pays, Coordinated Care Harvest Bucks and eyeglass benefit at CoordinatedCareHealth.com/benefits.
(Note: My Health Pays—members begin earning rewards on 7/1/24, but may experience a delay in receiving rewards earned in the first few months due to system configurations.)
Will the Apple Health Expansion program mirror Medicaid benefits (both medical and behavioral health)?
Apple Health Expansion will mirror most Apple Health (Medicaid) benefits for physical health care including pharmacy and behavioral health care services.
Apple Health Expansion will not cover Health Homes; Intensive Behavioral Supportive Supervision; or any benefits operated by other state agencies including Intermediate Care Facilities (DSHS), Private Duty Nursing (DSHS/DDA), Behavioral Rehabilitative Services (DCYF), Medicaid Personal Care (DSHS), Community First Choice (DSHS), and HIV Case Management (DOH).
More information in the Provider Manual and Benefits Grid (PDF).
Are dental benefits included?
Dental benefits mirror Apple Health (Medicaid) for benefits available to adults ages 21+ and benefits available to young adults ages 19-20. Like Apple Health (Medicaid), services that are NOT medically necessary (e.g., cosmetic procedures) are not covered under Apple Health Expansion. Learn more about dental benefits on the Health Care Authority webpage and on Coordinated Care’s dental webpage.
What are the steps for getting an interpreter if one is needed?
Interpreter Services for provider visits and when calling Coordinated Care are available.
Providers may request an interpreter by:
- Option 1: Emailing the Interpreter Request form (PDF) to InterpreterRequests@centene.com.
- Option 2: Calling Provider Services and ask for an interpreter for the Apple Health Expansion member. Provider Services will ask a few intake questions and submit for scheduling. A scheduler will call back with the availability of interpreters to complete the scheduling.
Members may request an interpreter through their provider or Coordinated Care can assist.
- When members call Coordinated Care and need support in a language other than English or Spanish they can select “0” to get connected directly to our Member Services team and get support with an interpreter.
BILLING, PAYMENTS, PROVIDER PORTAL
Will Federally Qualified Health Centers (FQHCs) and Rural Health Centers (RHCs) receive enhancement payments for Apple Health Expansion?
No, FQHCs and RHCs will not receive the enhancement payments for AHE members. The one exception will be Tribal FQHCs.
Will the Apple Health Expansion population have any impact on Capitation agreements?
Members of Apple Health Expansion will be included in any Capitation payments.
What impact will the Apple Health Expansion population have on Value Based Agreements (VBAs) and P4P/P4Q programs?
The Apple Health Expansion population will not be included in VBA's or Pay for Performance (P4P) in 2024.
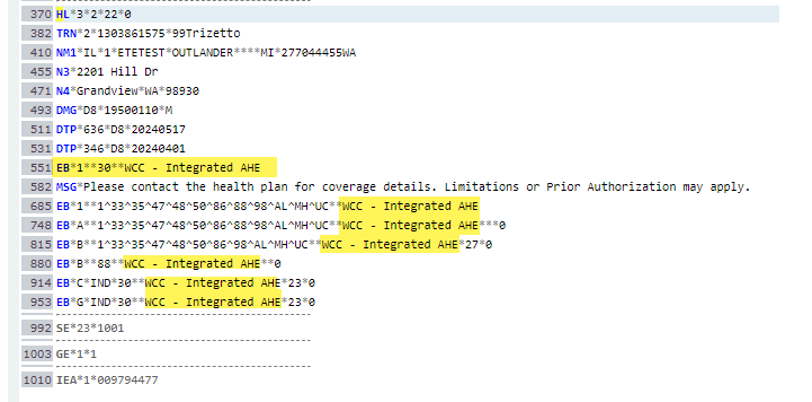
Will EEV 271 Response Plan Description show enrollees on this program & how will it display?
Please refer to the below screen shot for how it will display in 271.
How can Apple Health Expansion members be identified in Provider One (eligibility)?
Provider One will have Apple Health Expansion records in the MCO section, similar to how Behavioral Health Services Only benefits are displayed. Please see the screen shot below:
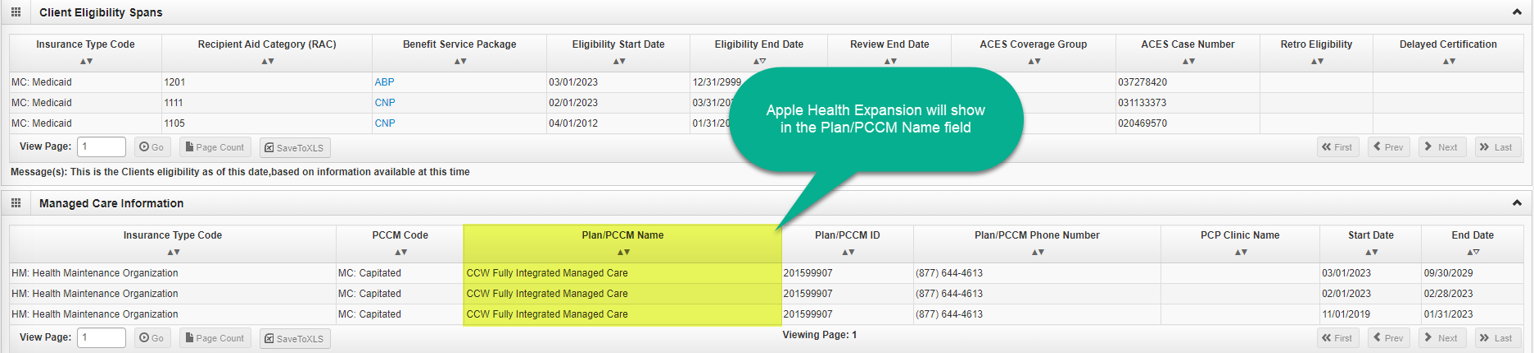
If you need information on using Provider One, the HCA website has more information located here.
How can Apple Health Expansion members be identified in the Coordinated Care Provider Portal?
In the Coordinated Care Provider Portal, the individual patient eligibility check result screen will display in the “Product Name” field. Please see screen shot below:
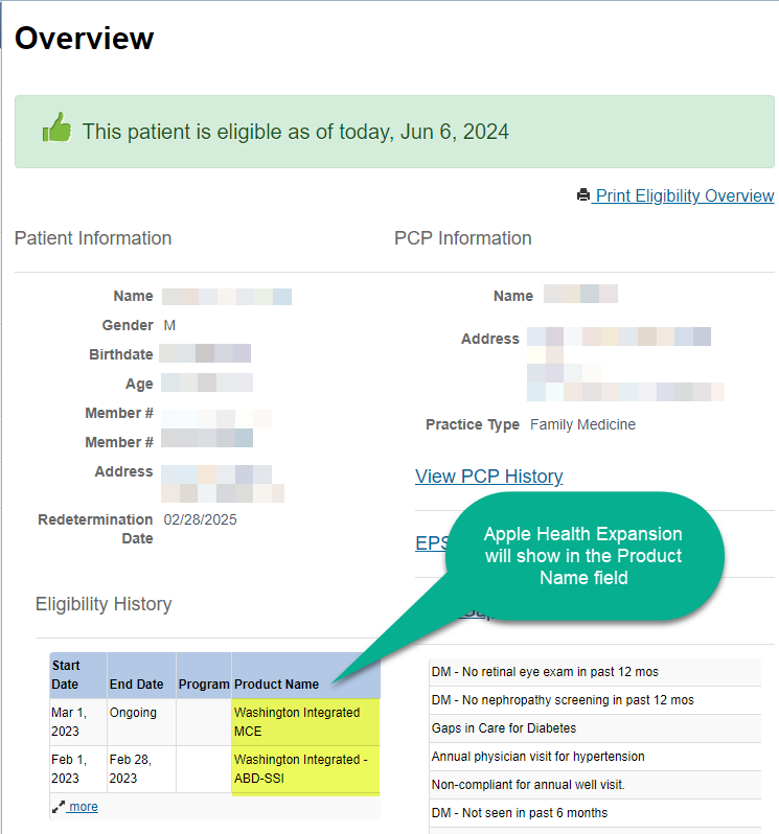
Primary Care Physicians (PCPs), can also see this information in the downloaded Patient Roster where Apple Health Expansion will be indicated in the Plan product field.
HCA RESOURCES
HCA Communications toolkit (PDF)
HCA Apple Health Expansion provider page
______________________________________________________________________________________
General Updates
Updated Apple Health client forms: Medical Equipment and Supplies and Outpatient Rehabilitation
Attention providers: Apple Health (Medicaid) client forms required for certain Medical Equipment and Supplies and Outpatient Rehabilitation Extension Requests are available for use.
Prior Authorization and equipment proof of delivery requirements
HCA has updated Apple Health (Medicaid) client forms related to Medical Equipment and Supplies and Outpatient Rehabilitation. Forms can be found here. The following forms have been updated and are available for use:
- HCA Prescription / Standard Written Order Form 13-794
- Outpatient Rehabilitation Limitation Extension Request Form 13-786
- Hospital Bed Evaluation Form 13-747
- Bathroom Equipment Form 13-872
- Speech & Language Pathologist Evaluation for Speech Generating Device Form 13-0127
Billing Guide and Fee Schedule
HCA will revise the Medical Equipment & Supplies Billing Guide to reflect this change. See HCA’s Provider billing guides and fee schedules, under Medical Equipment & Supplies effective July 1, 2024.
SELF NOMINATION NOW OPEN FOR 2024 IMMUNIZE WA AWARDS
The Immunize WA awards, recognizing clinics that achieve immunization coverage criteria for childhood, adolescents, and now HPV dose initiation for 9- and 10-year-olds, celebrates its 10-year anniversary in 2024!
Nominations are now open!
Providers must self-nominate during June 1 and July 15, 2024. The 2024 award recipients will be announced on August 20, 2024, during National Immunization Awareness Month.
To nominate your clinic for Immunize WA:
- A short video on how to run your coverage rate report can be found here.
- Coverage rate report can be found here (PDF).
- Complete the nomination form here.
- Submit your coverage rate report to immunizewa@doh.wa.gov.
- Please include your VFC pin in the subject line.
Don't miss the opportunity to nominate yourself/your clinic! Nominations run through July 15, 2024. More information can be found on the Immunize WA web page here.
Occupational therapy for behavioral health conditions - Fact Sheet Feb 2024
Work has continued on the implementation of 2023 legislation SB 5228 requiring the Health Care Authority (HCA) to expand coverage within Apple Health (Medicaid) to ensure that licensed behavioral health agencies (BHA) are reimbursed by managed care organizations (MCO) for the medically necessary occupational therapy needs of their clients by July 1, 2024.
Updates have been made to the occupational therapy for behavioral health conditions fact sheet and can be found here (PDF). The intent of this fact sheet is to provide guidance for behavioral health agencies (BHA) who want to add occupational therapy treatment services covered by Apple Health beginning July 1, 2024. For managed care, the expectation of the increased per member per month was incorporated into the physical health side of the rates as a program adjustment beginning July 1, 2024. For calendar year 2025, the rates for services will be included on the behavioral health side after there is sufficient data to analyze services for adjustments to be made. For Behavioral Health Services Only (BHSO) clients, bill fee-for-service (FFS) for dates of service 07/01/2024 – 12/31/2024. For dates of service starting on or after 01/01/2025, services must be billed to the appropriate managed care plan for BHSO services.
______________________________________________________________________________________
Quality
Medicaid Quality
ADHD Follow Up on Kids
Children with new prescription for ADHD medication should receive a follow up visit within 30 days of starting the medication.
Asthma and 90 Day Medication Refills
Moving members with asthma prescriptions to 90-day medication refills may increase their maintenance medication adherence.
Mammograms (HEDIS Measure)
The HEDIS measure assesses women ages 50-74 who had at least one mammogram to screen for breast cancer in the past 2 years.
Telehealth
Telehealth increases access to physicians and specialists to help patients receive the right care, at the right place, at the right time.
More information:
Antidepressant Medication Management (HEDIS Measure)
The HEDIS measure assess adults 18 years of age and older with a diagnosis of major depression who were newly treated with antidepressant medication and remained on their antidepressant medications.
Wellcare Quality
Men’s Health Month in June encourages males to implement healthy lifestyle decisions to improve their overall health. Many diseases like heart disease and cancer disproportionately impact men but are preventable through regular doctor’s visits and healthy lifestyle choices.
According to the US Department of Health and Human Services’ Office of Minority Health, US men in general are expected to live nearly six years less than women, and non-Hispanic Black and American Indian/Alaska Native men have a lower life expectancy than non-Hispanic white men.
The following resources can be utilized for information about preventive services covered by Medicare, including:
- Alcohol misuse screening and counseling
- Cancer screening:
- Cardiovascular Disease
- Counseling to prevent tobacco use
- IBT for obesity
Find out when your patient is eligible for services here (PDF). If you need help, contact your eligibility service provider.
______________________________________________________________________________________
Payment & Clinical Policy Updates
Clinical Policy Updates
The below policies were updated as part of our regular monthly review in May. The policy changes are effective July 1, 2024. You will find the policies, including a description of the revisions, posted on the policy site.
Policy Number | Policy Title | Line of Business |
WA.CP.MP.27 | Hyperbaric Oxygen Therapy | Apple Health |
WA.CP.MP.504 | Elective Deliveries Before 39 Weeks | Apple Health |
WA.CP.MP.513 | Cardiac Stents | Apple Health |
WA.CP.MP.519 | Administrative Days | Apple Health |
WA.CP.BH.528 | Intensive Behavioral Supportive Supervision | Apple Health |
WA.CP.BH.529 | Community Behavioral Health Support - Supportive Supervision | Apple Health |
HIM.CP.BH.500 | Behavioral Health Treatment Documentation | Ambetter |
CP.MP.101 | Donor lymphocyte infusion | Apple Health & Ambetter |
CP.MP.160 | Implantable Wireless Pulmonary Artery Pressure Monitoring | Ambetter |
CP.MP.170 | Nerve Blocks and Neurolysis for Pain Management | Apple Health & Ambetter |
CP.MP.182 | Short Inpatient Hospital Stay | Apple Health & Ambetter |
CP.MP.246 | Pediatric Kidney Transplant | Apple Health & Ambetter |
CP.MP.57 | Lung Transplantation | Apple Health & Ambetter |
The below policies were updated as part of our regular monthly review in May. The policy changes are effective October 1, 2024. You will find the policies, including a description of the revisions, posted on the policy site.
Policy Number | Policy Title | Line of Business |
CP.MP.176 | Outpatient Cardiac Rehabilitation | Ambetter |
CP.BH.201 | Deep TMS for OCD | Ambetter |
The below policies were previously announced as revised on the date noted. You will find the policies posted on the policy site.
Policy Number | Policy Title | Effective Date | Line of Business |
CP.MP.22 | Stereotactic Body Radiation Therapy | 7/1/24 | Apple Health & Ambetter |
CP.MP.62 | Hyperhidrosis Treatments | 7/1/24 | Apple Health & Ambetter |
CP.MP.82 | NICU Apnea Bradycardia Guidelines | 7/1/24 | Apple Health & Ambetter |
CP.MP.173 | Implantable Intrathecal or Epidural Pain Pump | 7/1/24 | Apple Health & Ambetter |
CP.MP.190 | Oxygen Use and Concentrators | 7/1/24 | Ambetter |
CP.MP.243 | Implantable Loop Recorder (Implantable Cardiac Monitor) | 7/1/24 | Apple Health & Ambetter |
CP.MP.248 | Facility Based Sleep Studies for Obstructive Sleep Apnea | 7/1/24 | Apple Health & Ambetter |
WA.CP.MP.521 | Behavioral Health Wraparound Support (BHWS), previously Behavioral Health Personal Care Services | 7/1/24 | Apple Health |
CP.MP.40 | Gastric Electrical Stimulation | 9/1/24 | Apple Health & Ambetter |
CP.MP.91 | Obstetrical Home Health Care Programs | 9/1/24 | Ambetter |
CP.MP.132 | Heart-Lung Transplant | 9/1/24 | Apple Health & Ambetter |
CP.MP.141 | Non-Myeloablative Allogenic Stem Cell Transplants | 9/1/24 | Apple Health & Ambetter |
CP.MP.185 | Skin and Soft Tissue Substitutes for Chronic Wounds | 9/1/24 | Ambetter |
WA.CP.MP.185 | Skin and Soft Tissue Substitutes for Chronic Wounds | 9/1/24 | Apple Health |
Payment Policy Updates
The below policy was updated as part of our regular monthly review in May. The policy changes are effective July 1, 2024. You will find the policy, including a description of the revisions, posted on the policy site.
Policy Number | Policy Title | Line of Business |
CC.PP.206 | Skilled Nursing Facility Leveling | Apple Health & Ambetter |
______________________________________________________________________________________
Pharmacy Updates
Non-Contracted Drugs Update- Apple Health Expansion
Beginning 07/01/2024, Apple Health Expansion coverage will become effective as a state funded medical assistance program to uninsured adults who meet certain requirements.
Pharmacy coverage will be mostly the same as Apple Health (Medicaid) except for select drugs that will need to be billed to the Washington State Health Care Authority. Those drugs include many of the oral HIV products, Oncology, and Cystic Fibrosis Agents. There will be a reject message at point of sale that states, “Bill to Health Care Authority. Contact HCA at 800-562-3022.”
The preferred drug list will be available on our Pharmacy page.
Hyaluronic Acid Coverage Change Reminder
Effective 7/1/2024, as instructed by the Washington State Health Care Authority, Coordinated Care will no longer cover hyaluronic acid products. This is based upon the review of evidence performed by the Health Technology Clinical Committee.
Code | Description of Codes |
J7320 | Hyaluronan or derivitive, GenVisc 850, for intra-articular injection, 1 mg |
J7321 | Hyaluronan or derivative, hyalgan, Supartz or VISCO-3, for intra-articular injection, per dose |
J7322 | Hyaluronan or derivative, Hymovis, for intra-articular injection, 1 mg |
J7323 | Hyaluronan or derivative, euflexxa, for intra-articular injection, per dose |
J7324 | Hyaluronan or derivative, Orthovisc, for intra-articular injection, per dose |
J7325 | Hyaluronan or derivative, synvisc or Synvisc-One, for intra-articular injection, 1 mg |
J7326 | Hyaluronan or derivative, Gel-One, for intra-articular injection, per dose |
J7327 | Hyaluronan or derivative, Monovisc, for intra-articular injection, per dose |
J7328 | Hyaluronan or derivative, gelsyn-3, for intra-articular injection, 0.1 mg |
J7332 | Hyaluronan or derivative, Synojoynt, for intra-articular injection, 1 mg |
J7332 | Hyaluronan or derivative, TRILURON, for intra-articular injection, 1 mg |
______________________________________________________________________________________
Training/Education
Childhood Development & the Impact of Trauma This training provides information on key areas of childhood development; social, cognitive, and physical development are all explored. The training focuses on how complex trauma affects development in infants and toddlers, school aged children, and adolescents. Facilitated by Zia Freeman, MA, LMHC, Community Educator with Coordinated Care. When: Jul 10, 2024, 01:00 PM Register here.
Commercial Sexual Exploitation of Children (CSEC) Responding to Sexual Exploitation and Trafficking of Youth was developed by Leslie Briner, MSW of Youth Care; This training will prepare caregivers and service providers to identify, engage and provide support to sexually exploited youth; Introductory topics include definitions, language, landscape of exploitation, identification including “red flags”, victim engagements and interventions. Jul 11, 2024, 10:00 AM Register here.
Childhood Development & the Impact of Trauma This training provides information on key areas of childhood development; social, cognitive, and physical development are all explored. The training focuses on how complex trauma effects development in infants and toddlers, school aged children, and adolescents. Jul 17, 2024, 01:00 PM – 02:30 Register here.
Resiliency Coordinated Care’s Resilience Training provides information on how to foster resilience in children. It reviews research from Ann Masten and Laurence Gonzales to guide discussion. This training looks at factors that affect resilience, the human adaptive process, ways to successfully cope with trauma, and the 12 steps of successful survivors. The training ends with a discussion around how caregivers can help their children feel safe, capable and loveable. Jul 18, 2024, 11:00 AM Register here.
Trauma Informed Care: Being an Advocate for the Youth you serve. Children with a background of trauma may need to have several advocates to help them. Becoming an advocate for the youth you serve and care for can be invaluable to a young person in the child welfare system. This webinar provides guidance on: Working with the team members involved, helping others understand the child and trauma informed care, consider treatment modality basics and when to question treatment and Caring for your own needs. Facilitated by Zia Freeman, MA, LMHC Community Educator with Coordinated Care Jul 26, 2024, 01:00 – 02:30 Register here.

