February 2023 Provider News
Date: 02/28/23
In this issue:
- General Updates - PaySpan and Continuity of Care Provider Payments
- Quality - Medicaid: February Heart Health Month, Lead Screening, Asthma 90 Day Refill, Clinical Practice Guidelines, Wellcare: Annual Wellness Visits, Visit Coding, Diagnosis and Billings
- Tribal - Enroll for EFT/ERA with PaySpan- open to all IHCP's
- Payment & Clinical Policy - Interventional Pain Management Updates, Monthly Updates
- Wellcare - New Century Health Oncology Prior Authorization List
- Apple Health Core Connections - TF-CBT Training
- Training/Education - Centene’s Clinical Provider Training, Committing to Action: Facilitators and Barriers to Achieving Equity, Motivational Interviewing, 2023 Washington Behavioral Healthcare Conference
______________________________________________________________________________________
General Updates
Continuity of Care provider payments for Centene will be administered via Payspan going forward. We wanted to make you are aware that Payspan offers monthly training webinars for providers. These webinars cover the registration process for both electronic funds transfers as well as registering and navigating the Payspan portal where providers will be able to view their explanation of payments. Below is a list of upcoming training dates along with the registration link. The next training is scheduled for February 15, 2023. For additional support, providers can contact the Payspan call center at 1-877-331-7154 (ext. 1), Monday-Friday between the hours of 8am-8pm ET.
Payspan Webinar Dates:
- Mar 15, 2023 | 1:30PM - 3:00PM EDT
- Apr 19, 2023 | 1:30PM - 3:00PM EDT
- Apr 19, 2023 | 5:30PM - 7:00PM EDT
- May 17, 2023| 1:30PM - 3:00PM EDT
- Jun 21, 2023 | 1:30PM - 3:00PM EDT
______________________________________________________________________________________
Quality
Medicaid Quality
February – American Heart Health Month
CDC Foundation’s “Live to the Beat” campaign focuses on encouraging black adults ages 35 to 54 to take small steps in reducing risks to cardiovascular disease. Using this website’s tool assists your patients in learning how to control their blood pressure, manage cholesterol, and blood glucose levels, move more and eat healthier, stress less, work with their health team, and quit smoking.
Lead Poisoning Screening - EPSDT
All children 12 – 24 months of age should be tested for the risk of lead poisoning. This testing is a federally mandated preventative health benefit and uses traditional, folk, ethnic remedies, or cosmetics. (Examples: Greta, Azarcon, Ghasard, Ba-baw-san, Sindoor and Kohl).
Asthma and 90 Day Refills
Moving members with asthma to 90-day refills may increase their medication adherence. Coordinated Care provides members with 90-day supplies through our preferred mail order pharmacy, CVS Caremark, or any contracted pharmacy.
Clinical Practice Guidelines
Reminder that the Preventative and Clinical Practice Guidelines are on the Provider Website (last review April 2022).
You can review them on our Preventative and Clinical Practice Guidelines page.
Wellcare Quality
February marks Black History Month, a time to honor the important contributions that Black Americans have made and to recognize their sacrifices. This tradition that got its start in the Jim Crow era and was officially recognized in 1976 as part of the nation's bicentennial celebrations.
This month, the Centers for Medicare & Medicaid Services Office of Minority Health (CMS OMH) celebrates both American Heart Month and Black History Month (https://www.cms.gov/about-cms/agency-information/omh/resource-center/health-observances). According to the Centers for Disease Control & Prevention (CDC), and the National Heart, Lung and Blood Institute, one person dies every 34 seconds from heart disease, which is the leading cause of death for both men, women, and most racial and ethnic groups in the U.S.
Research shows that disparities persist as Black adults continue to experience higher death rates than white adults, especially in rural or segregated areas. Black people also have the highest prevalence of cardiovascular disease out of all racial groups in the U.S., Black women have the highest percentage of high blood pressure compared to other groups. Nearly 58% of Black women over age 20 have high blood pressure. If high blood pressure remains uncontrolled, it increases a person’s risk for heart disease, stroke, heart failure, kidney disease and cognitive decline later in life.
Visit National Heart, Lung, and Blood Institute for Dietary Approaches to Stop Hypertension (DASH).
Black communities are often disproportionately affected by heart disease and many of its risk factors based on certain social determinants of health, including access to medication, preventive services, and safe exercise. CMS OMH hopes to highlight the importance of heart disease prevention and care management to combat health disparities in Black communities, who often have increased risk of cardiovascular disease (CVD).
About 297,000 Washington State residents have coronary heart disease, the most common form of heart disease that can often be prevented by eating healthier, getting enough sleep, stress reduction and quitting smoking.
Annual Wellness Visits:
Annual Wellness Visits (AWV) are an opportunity to close clinical HEDIS measure gaps, establish or strengthen your Provider/Patient rapport and most importantly provide quality health care including early detection to save lives. The AWV helps develop or update a Personalized Prevention Plan (PPP) and perform a Health Risk Assessment (HRA).
Resources for Annual Wellness Visits: helpful resource tools for the AWV can be found here.
CMS website Medicare Learning Network documents 12 defined components of the First Annual Wellness Visit and subsequent Annual Wellness Visits having 11 components. Preparing eligible Patients for the AWV can include encouraging them to bring to their appointment at a minimum:
- Medical records, including immunization records
- Detailed family health history
- Full list of medications and supplements, including calcium and vitamins, and how often and how much of each they take
- Full list of current providers and suppliers involved in their care, including community-based providers (for example, personal care, adult day care, and home-delivered meals), and behavioral health specialists
Annual Wellness Visit Coding, Diagnosis and Billings
Resources by the Medical Learning Network can be found here.
Coding
CMS website Medicare Learning Network documents use of these HCPCS codes to file AWV claims:
G0438
Annual wellness visit, includes a personalized prevention plan of service (PPS), initial visit
G0439
Annual wellness visit, includes a personalized prevention plan of service (PPS), subsequent visit
G0468*
Federally qualified health center (FQHC) visit, IPPE or AWV; a FQHC visit that includes an initial preventive physical examination (IPPE) or annual wellness visit (AWV) and includes a typical bundle of Medicare-covered services that would be furnished per diem, to a patient receiving an IPPE or AWV
* Section 60.2 of Medicare Claims Processing Manual, Chapter 9, has more information on how to bill HCPCS code G0468.
Diagnosis
CMS website Medicare Learning Network documents a diagnosis code must be reported when submitting AWV claims. “We don’t require you to use a specific AWV diagnosis code, so you may choose any diagnosis code consistent with the patient’s exam.”
Billing
Part B covers an AWV if performed by a:
- Physician (doctor of medicine or osteopathy)
- Qualified non-physician practitioner (NPP) (physician assistant [PA], nurse practitioner [NP], or certified clinical nurse specialist [CCNS])
- Medical professional (including health educator, registered dietitian, nutrition professional, or other licensed practitioner), or a team of medical professionals that a physician directly supervises
"When you provide an AWV and a significant, separately identifiable, medically necessary Evaluation and Management (E/M) service, we may pay for the additional service. Report the additional CPT code with modifier –25. That portion of the visit must be medically necessary and reasonable to treat the patient’s illness or injury or to improve the functioning of a malformed body part.
You can only bill G0438 or G0439 once in a 12-month period. G0438 is for the first AWV and G0439 is for subsequent AWVs. Remember, you must not bill G0438 or G0439 within 12 months of a previous G0402 (IPPE) billing for the same patient. We deny these claims with messages of, “Benefit maximum for this time period or occurrence has been reached” and “Consult plan benefit documents/guidelines for information about restrictions for this service.”
CMS website Medicare Learning Network documents Medicare telehealth as including HCPCS codes G0438 and G0439. List of Telehealth Services webpage has more information.
Advance Care Planning as an Optional Annual Wellness Visit Element resources as documented by CMS Medical Learning Network.
CMS website Medicare Learning Network documents Advance Care Planning (ACP) as the face-to-face conversation between a physician (or other qualified health care professional) and a patient to discuss their health care wishes and medical treatment preferences if they become unable to communicate or make decisions about their care. At the patient’s discretion, you can provide the ACP during the AWV.
Coding
CMS website Medicare Learning Network documents use of these CPT codes to file ACP claims as an optional AWV element:
99497
Advance care planning including the explanation and discussion of advance directives such as standard forms (with completion of such forms, when performed), by the physician or other qualified health care professional; first 30 minutes, face-to-face with the patient, family member(s), and/or surrogate
99498
Advance care planning including the explanation and discussion of advance directives such as standard forms (with completion of such forms, when performed), by the physician or other qualified health care professional; each additional 30 minutes (List separately in addition to code for primary procedure)
Diagnosis
CMS website Medicare Learning Network documents “You must report a diagnosis code when submitting an ACP claim as an optional AWV element. We don’t require you to use a specific ACP diagnosis code as an optional AWV element, so you may choose any diagnosis code consistent with a patient’s exam”.
Billing
CMS website Medicare Learning Network documents “Medicare will waive both the Part B ACP coinsurance and deductible” when:
- Provided on the same day as the covered AWV
- Provided by the same provider as the covered AWV
- Billed with modifier –33 (Preventive Service)
- Billed on the same claim as the AWV
As documented on the MLN, Medicare will waive the ACP deductible and coinsurance once per year when billed with the AWV. If there is a denial of the AWV billed with ACP for exceeding the once-per-year limit, Medicare applies the ACP deductible and coinsurance.
Medicare will apply the deductible and coinsurance when you deliver the ACP outside of the covered AWV. The MLN documents there are no limits on the number of times you can report ACP for a certain patient in a certain time period. It is further documented when billing this service multiple times, to document changes in the patient’s health status or wishes about their end-of-life care.
e-Code of Federal regulations pertaining to AWV
CPT only copyright 2021 American Medical Association. This information is for reference and should be verified by the user on the official CMS website.
______________________________________________________________________________________
Tribal
Enroll for EFT/ERA with PaySpan- open to all IHCP's
All Indian Health Care Providers (IHCP's), regardless of contract status, are able to enroll with PaySpan to get access to EFT/ERA. PaySpan is our partner for web based electronic fund transfer (EFT) and electronic remittance advices (ERA).
Use this link for more information on how to enroll today or contact your Provider Relations rep for additional assistance.
______________________________________________________________________________________
Payment & Clinical Policy
Clinical Policy
Interventional Pain Management Updates
Effective June 1, 2023, interventional pain management services will be reviewed by National Imaging Associates, Inc. (NIA) to determine if the services are medically necessary and covered under Coordinated Care health plans. You will find the policies on the NIA Website. A link is available under “Provider Resources” on CoordinatedCareHealth.com. Policy names are listed below under Monthly Updates.
CPT codes considered interventional pain management for purposes of this review are: 0213T-0218T, 0228T-0231T, G0260, 27096, 62320-62323, 64479, 64480, 64483, 64484, 64490-64495, 64633-64636. All codes currently require prior authorization, but effective 6/1/23, authorization will be provided by NIA.
Monthly Updates:
The below clinical policies received updates as part of our regular monthly review in December. These policy changes are effective XXX, 2023. You will find the policies, including a description of the revisions, posted on the policy site.
Policy Number | Policy Title | Line of Business |
|---|---|---|
| NIA.CG.300 | Epidural Spine Injections | Apple Health & Ambetter |
| NIA.CG.301 | Facet Joint Injections | Apple Health & Ambetter |
| NIA.CG.302 | Facet Joint Denervation | Apple Health & Ambetter |
| NIA.CG.305 | Sacroiliac Join Injection | Apple Health & Ambetter |
Miscellaneous Updates:
The below policy was updated by NIA and reviewed as part of our regular monthly review in February. The policy changes are effective March 1, 2023. You will find the policy, including a description of the revisions, posted on the NIA Website. A link is available under “Provider Resources” on CoordinatedCareHealth.com. Policy names are listed below under Monthly Updates.
| Policy Number | Policy Title | Effective Date | Line of Business |
|---|---|---|---|
NIA.CG.062 | CT Coronary Angiography (CCTA) | 3/1/23 | Apple Health & Ambetter |
Monthly Updates:
The below clinical policies received updates as part of our regular monthly review in February. These policy changes are effective March 1, 2023. You will find the policies, including a description of the revisions, posted on the policy site.
| Policy Number | Policy Title | Line of Business |
|---|---|---|
CP.BH.500 | Behavioral Health Treatment Document Requirements | Apple Health & Ambetter |
| CP.BH.201 | Deep Transcranial Magnetic Stimulation for Treatment of Obsessive Compulsive Disorder | Ambetter |
| WA.CP.MP.515 | Fecal Microbiota Transplantation | Apple Health |
| WA.CP.MP.95 | Gender Affirming Procedures | Ambetter |
| CP.MP.136 | Home Births | Apple Health & Ambetter |
| CP.MP.62 | Hyperhidrosis Treatments | Apple Health & Ambetter |
| CP.MP.173 | Implantable Intrathecal or Epidural Pain Pump | Apple Health & Ambetter |
| CP.MP.190 | Outpatient Oxygen Use | Ambetter |
| WA.CP.MP.248 | Sleep Apnea Diagnosis and Treatment | Apple Health & Ambetter |
| WA.CP.MP.526 | Stem Cell Therapy for Musculoskeletal Conditions | Apple Health |
| CP.MP.22 | Stereotactic Body Radiation Therapy | Apple Health & Ambetter |
| CP.BH.100 | Substance Use Treatment and Services | Apple Health & Ambetter |
| CP.MP.162 | Tandem Transplant | Apple Health & Ambetter |
| WA.CP.MP.510 | Tinnitus Treatment | Apple Health |
The below policies were updated as part of our regular monthly review in February. The policy changes are effective June 1, 2023. You will find the policies, including a description of the revisions, posted on the policy site.
| Policy Number | Policy Title | Effective Date | Line of Business |
|---|---|---|---|
CP.BH.104 | Applied Behavior Analysis | 6/1/23 | Apple Health & Ambetter |
| CP.BH.200 | Transcranial Magnetic Stimulation for Treatment Resistant Major Depression | 6/1/23 | Apple Health & Ambetter |
The below policy will be archived effective June 1, 2023. The policy will be replaced with a version of the policy with the same name but labeled CP.BH.104 which is available on the policy site.
| Policy Number | Policy Title | Line of Business |
|---|---|---|
WA.CP.BH.104 | Applied Behavior Analysis | Apple Health |
The below policies will be archived effective June 1, 2023. The policies will be replaced with NIA versions of the policies as described above.
| Policy Number | Policy Title | Effective Date | Line of Business |
|---|---|---|---|
CP.MP.164 | Caudal or Interlaminar Epidural Steroid Injections for Pain Management | 6/1/23 | Apple Health & Ambetter |
| CP.MP.171 | Facet Joint Interventions for Pain Management | 6/1/23 | Ambetter |
| WA.CP.MP.171 | Facet Joint Interventions for Pain Management | 6/1/23 | Apple Health |
| CP.MP.166 | Sacroiliac Joint Interventions for Pain Management | 6/1/23 | Apple Health & Ambetter |
| CP.MP.165 | Selective Nerve Root Blocks and Transforaminal Epidural Injections for Pain Management | 6/1/23 | Apple Health & Ambetter |
The below new policy was previously announced effective on the dates noted. You will find the policy posted on the policy site.
| Policy Number | Policy Title | Effective Date | Line of Business |
|---|---|---|---|
CP.MP.247 | Transplant Service Documentation Requirements | 5/1/23 | Apple Health & Ambetter |
The below policies were previously announced to have changes effective on the dates noted. You will find the policies, including a description of the revisions, posted on the policy site.
| Policy Number | Policy Title | Effective Date | Line of Business |
|---|---|---|---|
CP.MP.202 | Orthognathic Surgery | 3/1/23 | Apple Health & Ambetter |
| CP.MP.61 | IV Moderate Sedation, IV Deep Sedation and General Anesthesia for Dental Procedures | 3/1/23 | Ambetter |
| CP.MP.150 | Phototherapy for Neonatal Hyperbilirubinemia | 3/1/23 | Apple Health & Ambetter |
| CP.MP.145 | Electric Tumor Treating Fields | 4/1/23 | Ambetter |
| CP.MP.151 | Transcatheter Closure of Patent Foramen Ovale | 4/1/23 | Apple Health & Ambetter |
| CP.MP.180 | Implantable Hypoglossal Nerve Stimulation for Obstructive Sleep Apnea | 4/1/23 | Apple Health & Ambetter |
| CP.MP.107 | Durable Medical Equipment (DME) and Orthotics and Prosthetics Guidelines | 5/1/23 | Apple Health & Ambetter |
______________________________________________________________________________________
Wellcare Updates
New Century Health Oncology Prior Authorization List: Effective April 1, 2023
Wellcare has partnered with New Century Health (NCH) to implement a new oncology prior authorization program effective April 1, 2023: Oncology Pathway Solutions.
What is the Wellcare Oncology Pathway Solutions program?
The Wellcare Oncology Pathway Solutions program provides prior authorization management for infusible, injectable, and oral chemotherapy agents and supportive drugs — including symptom management drugs and radiation oncology. The program emphasizes and supports the selection of Preferred Pathways for patient care and is administered by NCH.
Download the Medical Oncology (PDF) procedure code list.
Download the Radiation Oncology (PDF) procedure code list.
Guidance on Card Effective Date for Legacy Wellcare Medicare ID Cards Affects: Legacy Wellcare Medicare ID cards only Starting with 2023 ID cards, we have removed the plan year and now print the “Card Effective Date” on the top section of the ID card.
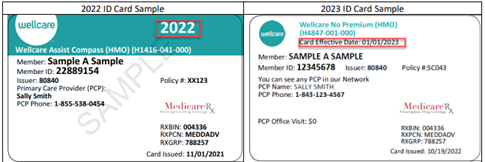
The Card Effective Date is not equivalent to the plan year that was listed on last year’s ID cards. The Card Effective Date is the date the member’s current coverage period began.
For existing members:
- Existing members that remained in the same plan for 2023 will be issued a replacement ID card with an effective date in the past (i.e., 1/1/2022 for a member that enrolled last year). These members can use their replacement ID card to access benefits now and at the start of the year.
- Existing members that rolled into a new plan in 2023 will be issued a replacement ID card with effective date in the future (i.e., 1/1/2023).
For new members:
- New members will have an effective date in the future (i.e., 1/1/2023 for new AEP enrollees)
Wellcare Medicare ID Card Effective Date Guidance
REMINDER of Wellcare Website and Portal Features:
Authorization Lookup Tool
From the Provider Tab, under the Tool sections, Providers can find the Authorization Lookup Tool. From this page providers can enter in CPT codes to find out if an authorization is needed and find additional authorization resources.
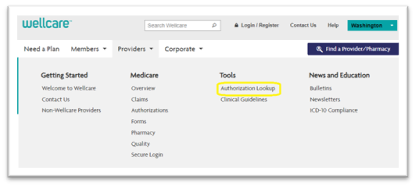
From the Authorization Lookup page select your line of business and enter a CPT to lookup authorization for services. This tool is for general information only. It does not take into consideration a specific member or contract agreement.
______________________________________________________________________________________
Apple Health Core Connections
Coordinated Care is the single managed care organization to administer the Integrated Managed Care Apple Health Foster Care program in collaboration with the Health Care Authority and Department of Children Youth and Families. This program serves children and youth in foster care, adoption support, alumni of foster care (ages 18-26), and children reunified with their parents. Coordinated Care’s program is named “Apple Health Core Connections.” You can reach us at 1-844-354-9876 or AHCCTeam@coordinatedcarehealth.com.
The Coordinated Care Community Education Team serves providers and their staff with training to support the needs of the Medicaid population. The CE Team can offer training on topics such as SBIRT, Adoption Success, Trauma Informed Care, ACEs, Resilience, and Secondary Trauma and Self Care. To request more information or to schedule no-cost training please email: communityeducation@coordinatedcarehealth.com
Trauma Focused Cognitive Behavioral Therapy
Coordinated Care is providing a no-cost Trauma-Focused Cognitive Behavioral Therapy (TF-CBT) Training for contracted, in-network Coordinated Care providers. This training will be held on Wednesday Mar 22 and Thursday Mar 23, 2023, from 8:30 a.m. to 5:00 p.m. Pacific time each day at: Confluence Technology Center, Wenatchee, WA. For more information reach out to Lindsey.C.Greene@coordinatedcareheatlh.com. Register here.
______________________________________________________________________________________
Training/Education
Visit Centene’s Clinical Provider Training website to find webinar events available to all Coordinated Care providers. Webinars are on clinical behavioral health topics and usually offer free continuing education hours. Click on the “National Provider Webinars” button on the right side of the page and scroll down to find a complete listing.
Foundation for Health Care Quality. Committing to Action: Facilitators and Barriers to Achieving Equity. In this webinar, representatives from different stakeholder groups within our health ecosystem discuss what committing to health equity looks like in their organization and how their work aligns with other current actions to improve equity within all of Washington state. March 9, 2023 from 12 to 1:30 pm. Register here.
Washington Foundation for Community Health. Motivational Interviewing. Training series in Spanish on February 23, March 2, March 9, and March 16, 2023. Register here.
2023 Washington Behavioral Healthcare Conference: Reconnect and Recharge. Registration opens April 1, 2023. Kennewick, WA June 14-16, 2023. Learn more here.

