August 2024 Provider News
Date: 08/28/24
In this issue:
- General Updates - Childhood Lead Poisoning Prevention, Telemedicine Policy Update
- Quality - Well-Child Visits & CDC highlighted Immunizations for August 2024, National Immunization Awareness Month, Wildfire Season CCW member FAQ, Asthma and 90 Day Medication Refills, Telehealth, Flouride, Hearing Loss
- Pharmacy Update - Fill Limit of 2 Fills per Month Effective 8/1/2024, International Overdose Awareness Day, Appropriate Use of GLP-1 Agonists
- Health Equity - Standard HE 3: Access and Availability of Language Services Element C
- Payment & Clinical Policy - Monthly Updates
- Training/Education - Upcoming Training Opportunities
______________________________________________________________________________________
General Updates
Childhood Lead Poisoning Prevention Program WA DOH
Federal regulations require that all children enrolled in Medicaid receive a blood lead test at 12 and 24 months of age, or at 24 to 72 months of age if no record of a previous test exists. The Department of Health (DOH) recommends screening all children not covered by Medicaid at 12 and 24 months of age using this algorithm (PDF).
More information can be found here.
Reach out with questions here: lead@doh.wa.gov
Telemedicine Policy Update
As of November 1, 2024, the teledermatology policy will end. If a provider would like to provide services via store and forward, HCA will continue to cover E-consult. The policy will be updated on November 1, 2024. Dermatologists can provide this consultative service, or they could provide services directly to the client in-person or via telemedicine.
______________________________________________________________________________________
Quality
Medicaid Quality
Well-Child Visits & CDC highlighted Immunizations for August 2024
Return to School: Who can Provide EPSDT Well-Child Checkups?
- Physicians and Resident Physicians
- Naturopathic Physicians
- Advanced Registered Nurse Practitioners (ARNPs)
- Physician Assistants (PAs)
- Registered Nurses working under the guidance of a Physician or ARNP may also perform EPSDT well-child checkups. More information.
National Immunization Awareness Month
National Immunization Awareness Month (NIAM) is an annual observance held in August to highlight the importance of vaccination for people of all ages. Together, we can help raise awareness about the importance of vaccination and encourage people to talk to a healthcare provider they trust about staying up to date on their vaccinations.
Use these resources to help you discuss vaccinations with your patients and parents during NIAM and throughout the year.
For Healthcare Professionals
All staff in healthcare practices, including non-clinical staff, play important roles during NIAM:
- Engage in learning opportunities with CDC’s Immunization Education and Training courses here.
- Make your practice a supportive space that welcomes vaccine questions and concerns from patients and parents. Resources here.
- Use proven strategies to encourage parents and patients to stay up to date on vaccinations. Resources here.
- Make immunization schedules easy for parents and patients to find by displaying them on your website.
- Use tools like PneumoRecs VaxAdvisor Mobile App to help you make vaccine recommendations.
- Share clear and accurate information about the latest vaccine recommendations, including COVID-19 vaccines and RSV vaccines.
* Providing vaccines at no cost to members under age 19. More information.
Return to School: Well-Child Outreach
Children are returning to in-person learning this fall. It is time to reach out and conduct catch up immunizations and well-childcare. Coordinated Care can provide a list of kids with critical care gaps.
Washington Wildfire Frequently Asked Questions (FAQs)
Whom can I contact if I have a question?
- Apple Health members: 1-877-644-4613 (TTY: 711);
- Staffed Monday-Friday 8:00am-5:00pm; urgent calls triage to Nurse Advice Line 24/7.
- Apple Health Core Connections: 1-844-354-9876 (TTY: 711);
- Staffed Monday-Friday 8:00am-5:00pm; urgent calls triage to Nurse Advice Line 24/7.
- 24-hour Nurse Advice Line: 1-877-644-4613.
The smoke is making my or my family member’s disease symptoms worse. Will someone be able to guide me where to go for care?
- If you or your loved ones have a lung or heart condition such as asthma, COPD or heart disease, or COVID-related symptoms, and are not able to refill or replace your medications, please call us at 1-877-644-4613 (TTY: 711). You can also ask to speak to a Registered Nurse who can help answer your healthcare questions.
- If you need to schedule or reschedule a doctor’s appointment or would like to speak with one of our professional Care Managers during this time of need, please call us at 1-844-237-6489. We can also help you with food, housing & transportation.
What if I have to leave my area and can’t visit my doctor or pharmacy to refill my prescription? Or, what if they are closed because of the fires?
- We have informed providers that out of network authorizations can be allowed.
- Prescriptions can be transferred and refilled at any network pharmacy.
- Early refills can be allowed if requested.
- We authorize pharmacies to provide up to a 90-day supply of medication when an emergency fill is needed.
I know that some services normally need an authorization request, such as early prescription refills. Which services still require a request during a wildfire?
- Some authorizations change status during a disaster, while others remain in effect. The list below describes what you need to know about certain services.
- Altered authorizations during a wildfire disaster:
- Pharmacies are instructed to allow early refills and up to a 90-day emergency medication supply if requested.
- Out of network provider visits.
- Authorizations needed during a wildfire disaster:
- Medical services or medication for medical necessity. We will process these requests as ‘urgent’ during a wildfire disaster.
- These changes will remain in effect until the emergency no longer exists, or 90 days after the emergency has been declared.
Will my doctor know that I may need to use a different source for
my prescription, or that I may need an early refill?
- We informed providers and pharmacies that early refills
and out of network authorizations can be allowed.
What should I do to keep my family healthy when a wildfire is in my area?
- Air quality can be poor from the wildfire smoke. Common symptoms include headache, dizziness, congestion, cough, runny nose, watery eyes, and shortness of breath.
- To avoid these symptoms, drink lots of water and stay indoors as much as possible. If possible, use air conditioning instead of opening windows to keep cool.
- If possible, use an air cleaner with a HEPA filter in order to create a ‘clean room.’ This room should not have a fireplace, and few windows or doors.
- Stock up on necessary medication and supplies stocked.
- Read more on how to protect your and your family's health from outdoor smoke.
Who is most at risk to wildfire smoke?
- Children under 18 and adults over 65.
- People with heart and lung diseases.
- People with illnesses and colds.
- People who have had a stroke.
- Pregnant women.
- People who smoke.
Additional resources from Coordinated Care and the State of Washington.
- Use our Teladoc service to see a doctor by phone or video from home at no cost. Go to CoordinatedCareHealth.com/Telehealth to get started.
- Governor Inslee’s Washington Wildfire Resources and Updates
- Washington Smoke Information Blog
- Washington State Department of Health
Asthma and 90 Day Medication Refills
Moving patients with asthma to 90-day refills may help increase their adherence to maintenance medication.
Telehealth
Telehealth increases access to physicians and specialists to help patients receive the right care, at the right place, at the right time.
More information:
Please refer to the following link for more information.
Fluoride - Health Professionals Fluoride and Healthful Diets
Wellcare Quality
Hearing Loss
Did you know? According to the National Institute of Health (NIH) Hearing aids reduce the rate of cognitive decline in high-risk dementia persons by almost 50% over a 3 year period. Screening and treating hearing loss can be a safe and effective tool for lowering dementia risks in all populations.
NIH-funded research team co-led by Dr. Frank Lin from Johns Hopkins University enrolled nearly 1,000 adults, ages 70 to 84, into a clinical trial. They compared the rate of cognitive decline over a three-year period between people who did and didn’t receive hearing aids.
The researchers recruited participants with substantial hearing loss from two different study populations. About 250 healthy older adults came from a long-term study of heart health which had more risk factors for developing dementia including advanced age and faster rates of cognitive decline.
Participants were randomly to one of two interventions. About half received hearing aids and instruction in how to use them. The other half were assigned to a health education program focused on promoting healthy aging.
People who received the hearing aids reported substantial improvement in communication abilities over the course of the study. Those in the health-education group, as expected, did not experience improvement in hearing and communication.
In all study participants, the researchers saw no difference in the rate of change in cognitive functioning between people who received the hearing aids and those who didn’t.
However, when the analysis focused on people from the heart-health study, who had a higher risk of dementia, the benefit of the hearing aids was substantial. Those who received hearing aids had an almost 50% reduction in the rate of cognitive decline compared with people in the health-education group.
The researchers are continuing to follow the study participants to see how changes in cognition develop over time. They’re also looking at brain scans and data on social engagement to better understand how protecting hearing may prevent cognitive decline in vulnerable older adults.
Study conclusions recommended for general health and well-being that older adults have their hearing checked regularly and any hearing issues properly addressed.
______________________________________________________________________________________
Pharmacy
Fill Limit of 2 Fills per Month Effective 08/01/2024
Effective 08/01/2024, a fill limit of 2 fills per month will be applied
to drugs in the following drug classes:
| Drug Class |
|---|
| MIGRAINE AGENTS: CALCITONIN GENE-RELATED PEPTIDE (CGRP) RECEPTOR ANTAGONISTS |
| ANTIANXIETY AGENTS: BENZODIAZEPINES |
| OPHTHALMIC AGENTS: IMMUNOMODULATORS |
| HEMATOPOIETIC AGENTS: IRON / IRON COMBINATIONS - ORAL |
| ANTIHYPERTENSIVES: ANTIADRENERGICS |
| ASTHMA AND COPD AGENTS: INHALED CORTICOSTEROID COMBINATIONS |
| ANTIHYPERLIPIDEMICS: PCSK-9 INHIBITORS |
| RESPIRATORY AGENTS: PULMONARY FIBROSING AGENTS |
When the fill limit is exceeded, these medications will reject with a point-of-sale message that states, “Use PA override type 8 and PAMC 28011004444 if more than 2 fills or drug is required.”
PA override type 8 with PAMC code 28011004444 may be submitted to process the claim under the following circumstances:
- The prescription is written for a short day’s day supply because the prescriber is monitoring the member’s supply.
- The member needs a take-home supply of medication for school, camp, or skilled nursing facility.
- For any other circumstance, the provider must acknowledge monitoring to provide justification that it is medically necessary for needing more than the allowable fill limit per month.
International Overdose Awareness Day
August 31 each year, International Overdose Awareness Day (IOAD) is a campaign to remember and grieve those who died, take action to encourage support and recovery, and help end overdose by spreading awareness about drug overdose prevention.
Appropriate Use of GLP-1 Agonists
GLP-1 agonists have become part of the standard of care in the treatment of Type II Diabetes. It is also important to note that coverage of GLP-1 agonists for weight loss indications are not covered as treatment of obesity is an excluded benefit.
Inappropriate prescribing of drugs indicated for the treatment of Type II Diabetes (such as Victoza, Ozempic and Mounjaro), when intended for treatment of obesity alone, has contributed to shortages of these products for patients with Type II diabetes.1,2 While these products have proven to be effective for their respective indications, they are not without side effects/adverse reactions. The most common side effects are gastrointestinal-related, including loss of appetite, nausea, vomiting, and diarrhea. Additional issues have been identified with patients needing surgery when taking these medications. Due to the delayed gastric emptying feature of these drugs, it has been reported (at least anecdotally) that patients may have increased risk of regurgitation and pulmonary aspiration during general anesthesia and deep sedation3. As a result, the American Society of Anesthesiologists have set guidelines for the holding GLP-1 agonists prior to elective procedures3.
- Semaglutide Injection
- Tirzepatide Injection
- American Society of Anesthesiologists Consensus-Based Guidance on Preoperative Management of Patients (Adults and Children) on Glucagon-Like-Peptide-1 (GLP-1) Receptor Agonists
______________________________________________________________________________________
Health Equity

Health Equity
Standard HE 3: Access and Availability of Language Services
Element C
Marketplace
Ambetter from Coordinated Care Health Plan Provider News Blast Copy
Member Language Demographics and Interpreter Resources for Marketplace
At Ambetter from Coordinated Care (Coordinated Care Corporation), our purpose is at the center of everything we do, which is Transforming the Health of the Community, One Person at a Time. Treating the whole patient is a major component of delivering quality healthcare and we recognize the importance of serving members in a culturally and linguistically appropriate manner.
Member Demographics and Our Members
Coordinated Care Corporation Health Plan members speak more than 15 languages. In 2020, 79.2% of Washington residents reported English as their preferred language, and 8.6% prefer Spanish, according to U.S. Census data.
Coordinated Care Corporation at a minimum conducts a language assessment on an annual basis to determine the current population language within the service area.
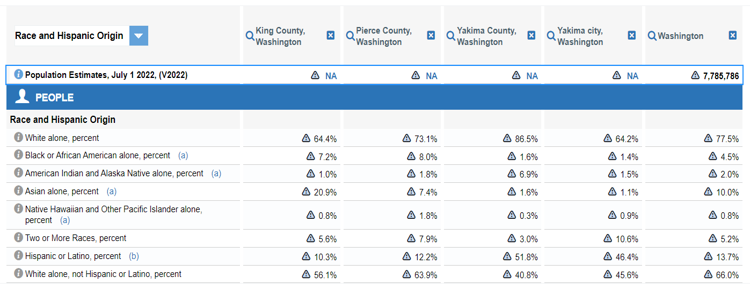
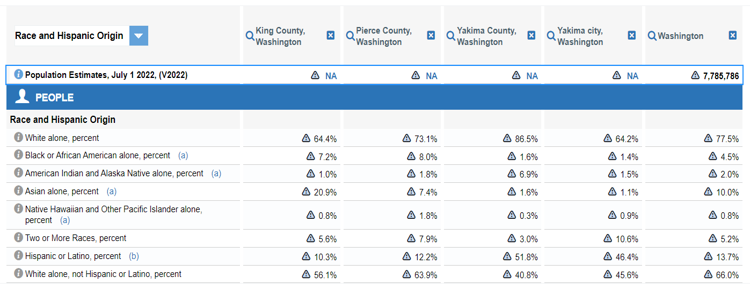
Census Data for King, Pierce, and Yakima counties in 2022:
Coordinated Care Corporation regularly looks at the following data to determine the needs of our members, future members, and the community. In 2023, 87.46% of Coordinated Care Corporation Marketplace members reported English as their preferred language, and 3.36% preferred Chinese.
| Languages Reported by Membership | Membership 2022 | Membership 2023 | ||
|---|---|---|---|---|
| f | % | f | % | |
| English | 27,533 | 87.80% | 59,818 | 87.46% |
| Chinese | 891 | 3.29% | 2,300 | 3.36% |
| Vietnamese | 636 | 2.03% | 1,424 | 2.08% |
| Spanish | 36 | .11% | 1,312 | 1.92% |
| Russian | 248 | .79% | 709 | 1.04% |
| Korean | 134 | .43% | 290 | 0.42% |
| Ukrainian | 46 | .15% | 187 | 0.27% |
| Panjabi | 70 | .22% | 166 | 0.24% |
| Arabic | 22 | .07% | 43 | 0.06% |
| Portuguese | 4 | .01% | 9 | 0.01% |
To find more information about the language preferences of your members, visit the Provider Portal. You are also encouraged to reach out to your dedicated Provider Engagement Administrator to learn more about how this information can be used to strengthen your relationship with your patients. For a list of provider engagement representatives by region navigate here or call the Customer Contact Center at 1-877-687-1197.
Translation and Alternate Formats of Documents Services
For members who require materials to be provided in an alternative format, Coordinated Care Corporation fulfills these requests including, but not limited to, audio format in original language of text, interpreter recording in member’s primary and/or preferred language, an interpreter may read the material to the member, or materials in hard copy braille format.
| Alternate Forms | 2022 | 2022 % of Total | 2023 | 2023 % of Total |
|---|---|---|---|---|
| SIGN LANGUAGES | 2 | .01% | 4 | .01% |
About the Americans with Disabilities Act
Disability is any substantial limitation of one or more of a person’s daily life activities and may be present from birth or may occur during a person’s lifetime. Any individual meeting any of these conditions is an individual with a disability for purposes of coverage under the Americans with Disabilities Act.
To meet Title VI of the Civil Rights Act of 1964 and Americans with Disabilities Act (ADA) health care providers are required to assure language access.
Programmatic access to healthcare means that policies and practices that are part of the delivery of healthcare do not hinder the ability of members with disabilities to receive the same quality of care as other persons.
In accordance with Title VI of the Civil Rights Act, Prohibition against national Origin Discriminations, the President’s Executive Order 131166, section 1557 of the Patient Protection and Affordable care Act, the Health Plan and its providers must make language assistance available to persons with Limited English Proficiency (LEP) at all points of contact during all hours of operation.
Overview of Interpreter Services
Language services are available at no cost to Ambetter members and providers without unreasonable delay at all medical points of contact. The member has the right to file a complaint or grievance if cultural and linguistic needs are not met.
Language services include:
- Telephonic services
- Oral translation (reading of English material in a members preferred language)
- In-person non-English interpretation
- American Sign language
- Auxiliary aids including alternate formats such as large print and braille
- Written translations for materials that are critical for obtaining health insurance coverage and access to health care services in non-English prevalent languages
Information is deemed to be critical for obtaining health insurance coverage or access to health care services if the material is required by law or regulation to provide the document to an individual.
To obtain language services for a member, contact Ambetter provider services at 877-687-1197.
For in person and American Sign Language requests, contact Ambetter Provider Services as soon as possible, or at least 5 business days before the appointment. All providers (Medical, Behavioral, Pharmacy, etc.) can request language services by calling our Provider Customer Contact Center at: 1-877-687-1197, TTY 711.
Restrictions Related to Interpretation or Facilitation of Communication:
- Providers may not request or require an individual with limited English proficiency to provide their own interpreter.
- Providers may not rely on staff other than qualified bilingual/multilingual staff to communicate directly with individuals with limited English proficiency.
- Providers may not use an accompanying adult or minor child to interpreter or facilitate communication.
Exceptions to these expectations include:
- In an emergency involving an imminent threat to the safety or welfare of an individual or the public where there is no qualified interpreter for the individual with limited English proficiency immediately available.
- Accompanying adults (minors are excluded) where the individual with limited English proficiency specifically requests that the accompanying adult interpret or facilitate communication, the accompanying adult agrees to provide such assistance, and reliance on that adult for such assistance is appropriate under the circumstances for minimal needs.
Providers are encouraged to document in the member’s medical record any member denial of professional interpreters and the circumstances that resulted in the use of a minor or accompanying adult as an interpreter.
Common Methods to Ensure Equal Communication and Access to Information:
- Provisions for intake forms to be completed by persons who are blind or with a low visual disability with the same confidentiality afforded other members:
- Use of large print forms, electronic or online web-based forms, or in-person staff assistance in a private location.
- Provision for a presence of sign language interpreters to enable full communication with deaf or hard of hearing members who use sign language.
- Provision for making auditory information (E.G., automated messages) available via alternative means:
- Written communication or secure web-based methods may be used as possible substitutes.
- Provision for communicating with deaf or hard of hearing members by telephone:
- Use of telephone relay services (TRS), video relay services (VRS), a TDD, or use of secure electronic means.
Cultural and linguistic availability of services is an important characteristic of the services Coordinated Care Corporation provides to its membership. Coordinated Care Corporation will continue to monitor, track, and trend all available data sources and is committed to ensuring that its policies and infrastructure are attuned to the diverse needs of all members.
Additional Language Resources
For additional help with language resources, refer to the Language Assistance page located here.
New Provider Orientation
To attend an upcoming New Provider Orientation or to request a one-on-one session online or in-person, visit the Coordinated Care Provider Events page for more information here.
To access the 2024 Provider & Billing Manual visit the Provider Resources page here and click on the link to the 2024 Provider & Billing Manual.
Our Provider Engagement Administrators are available to help you. For a list of provider engagement representatives by region, navigate here or call the Customer Contact Center at 1-877-687-1197.
To be removed from these fax notices or to request to be added to our email list for these notices, please reply to CoordinatedCareProvider@centene.com.

Health Equity
Standard HE 3: Access and Availability of Language Services
Element C
Medicaid
Coordinated Care of Washington, Inc., Health Plan Provider News Blast Copy
Member Language Demographics and Interpreter Resources for Medicaid
At Coordinated Care of Washington, Inc., (Coordinated Care), our purpose is at the center of everything we do, which is Transforming the Health of the Community, One Person at a Time. Treating the whole patient is a major component of delivering quality healthcare and we recognize the importance of serving members in a culturally and linguistically appropriate manner.
Member Demographics and Our Members
Coordinated Care members speak more than 15 languages. In 2020, 79.2% of Washington residents reported English as their preferred language, and 8.6% prefer Spanish, according to U.S. Census data.
Coordinated Care at a minimum conducts a language assessment on an annual basis to determine the current population language within the service area.
Census Data for King, Pierce, and Yakima Counties in 2022:
Coordinated Care regularly looks at the following data to determine the needs of our members, future members, and the community. In 2023, 80.84% of Coordinated Care Medicaid members reported English as their preferred language and 13.85% preferred Spanish.
| Languages Reported by Membership | Membership 2022 | Membership 2023 | ||
|---|---|---|---|---|
| f | % | f | % | |
| English | 191,971 | 78.61% | 168,697 | 80.84% |
| Spanish | 33,163 | 13.58% | 28,900 | 13.85% |
| Unknown | 4,481 | 1.83% | 264 | 0.13% |
| Russian | 1,844 | 0.76% | 2,019 | 0.97% |
| Vietnamese | 1,812 | 0.74% | 1,732 | 0.83% |
| Chinese | 1,402 | 0.57% | 801 | 0.38% |
| Ukrainian | 1,170 | 0.48% | 1,256 | 0.60% |
| Dari (Afghanistan) | 830 | 0.34% | 879 | 0.42% |
| Arabic | 644 | 0.31% | ||
To find more information about the language preferences of your members, visit the Provider Portal. You are also encouraged to reach out to your dedicated Provider Engagement Administrator to learn more about how this information can be used to strengthen your relationship with your patients. For a list of provider engagement representatives by region navigate here or call the Customer Contact Center at 1-877-687-1197.
Translation and Alternate Formats of Documents Services
For members who require materials to be provided in an alternative format, Coordinated Care fulfills these requests including, but not limited to, audio format in original language of text, interpreter recording in member’s primary and/or preferred language, an interpreter may read the material to the member, or materials in hard copy braille format.
| Alternate Forms | 2022 | 2022 % of Total | 2023 | 2023 % of Total |
|---|---|---|---|---|
| LARGE PRINT ENGLISH | 1,605 | 0.66% | 1,610 | 0.72% |
| SIGN LANGUAGES | 35 | 1.73% | 34 | 1.68% |
| BRAILLE (ENGLISH) | 35 | 2.18% | 29 | 1.80% |
About the Americans with Disabilities Act
Disability is any substantial limitation of one or more of a person’s daily life activities and may be present from birth or may occur during a person’s lifetime. Any individual meeting any of these conditions is an individual with a disability for purposes of coverage under the Americans with Disabilities Act.
To meet Title VI of the Civil Rights Act of 1964 and Americans with Disabilities Act (ADA) health care providers are required to assure language access.
Programmatic access to healthcare means that policies and practices that are part of the delivery of healthcare do not hinder the ability of members with disabilities to receive the same quality of care as other persons.
In accordance with Title VI of the Civil Rights Act, Prohibition against national Origin Discriminations, the President’s Executive Order 131166, section 1557 of the Patient Protection and Affordable care Act, The Health Plan and its providers must make language assistance available to persons with Limited English Proficiency (LEP) at all points of contact during all hours of operation.
Overview of Interpreter Services
Interpreter services are available in-person or by video or telephonic services through the Health Care Authority for Medicaid health care professionals to gain access to skilled and qualified spoken and sign language interpreters for Apple Health (Medicaid) clients who require access to quality, efficient language during their health care services.
The Interpreter Services program provides access to scheduling spoken and sign language interpreters at no additional cost to contracted providers. Spoken language and sign language requests have been separated to ensure clients receive an appropriate interpreter match.
Request Video or Telephonic Interpreter Services
- Request spoken language interpreters by visiting the Universal Language Service website at hcauniversal.com for more information.
Providers should be prepared to meet the needs of the hearing impaired.
Sign language interpreters are provided by master contracts through the Department of Enterprise Services (DES). The Office of the Deaf and Hard of Hearing (ODHH) oversees the master contracts and partners with HCA to improve access to Sign Language (SL) interpreters for Apple Health enrolled clients.
Request Sign Language Interpreters
- Request sign language interpreters through the Department of Enterprise Services (DES) Office of Deaf and Hard of Hearing (ODHH) master contract utilizing their online request system here.
Spoken Language Access Providers
Spoken language access providers (LAP) are provided through the HCA's spoken language contractor. They are required to be certified, authorized or recognized by Department of Social and Health Services Language Testing and Certification (DSHS-LTC) and provide services within the scope of practice as defined by the interpreter Code of Professional Conduct. Providers may not ask them to perform nonlanguage-related tasks.
Program eligibility requirements
In order for the Health Care Authority (HCA) to pay for interpreter services, the following criteria must be met:
- The client is an eligible Apple Health client.
- Services are covered under the client's benefit package.
- The health care provider is an enrolled HCA Medicaid provider.
HCA will not pay for interpreter services for:
- Inpatient hospital services
- Nursing facility services
- Administrative services
- Answering or responding to general phone inquiries or reminder calls
- Family member interpreters
- Other miscellaneous office tasks
Providers are encouraged to document in the member’s medical record any member denial of professional interpreters and the circumstances that resulted in the use of a minor or accompanying adult as an interpreter.
Additional Language Resources
ISpeak Cards
“ISpeak” cards help your members identify the preferred language when seeking care and are available to download and print from the Washington State Coalition for Language Access website at wascla.org. In addition to the ISpeak cards, you can also find a collection of materials, as well as a “Know Your Rights” flyer for help when using interpreter services in healthcare settings. These resources can be found here.
Cultural and linguistic availability of services is an important characteristic of the services Coordinated Care provides to its membership. Coordinated Care will continue to monitor, track, and trend all available data sources and is committed to ensuring that its policies and infrastructure are attuned to the diverse needs of all members.
Additional Language Resources
For additional help with language resources, refer to the Language Assistance Page located here.
New Provider Orientation
To attend an upcoming New Provider Orientation, the annual refresher training, or request a one-on-one session online or in person, visit the Coordinated Care Provider Events page for more information here.
To access the 2024 Provider Operations Manual visit the Provider Resources page here and select Apple Health (Medicaid) Manual and Guides, and select Provider Manual for Medicaid Foster Care & Apple Health Expansion (PDF).
Our Provider Engagement Administrators are available to help you. For a list of provider engagement representatives by region, navigate here or call the Customer Contact Center at 1-877-687-1197.
To be removed from these fax notices or to request to be added to our email list for these notices, please reply to CoordinatedCareProvider@centene.com.
______________________________________________________________________________________
Clinical Policy Updates
The below policies were updated as part of our regular monthly review in July. The policy changes are effective September 1, 2024. You will find the policies, including a description of the revisions, posted on the policy site.
| Policy Number | Policy Title | Line of Business |
|---|---|---|
| WA.CP.MP.514 | Extracorporeal Membrane Oxygenation Therapy | Apple Health |
| CP.BH.500 | Behavioral Health Treatment Documentation Requirements | Apple Health |
| CP.MP.14 | Cochlear Implant Replacements | Apple Health & Ambetter |
| CP.MP.48 | Neuromuscular Electrical Stimulation (NMES) | Ambetter |
| CP.MP.49 | Physical, Occupational and Speech Therapy Services | Apple Health & Ambetter |
| CP.MP.92 | Acupuncture | Ambetter |
| CP.MP.94 | Clinical Trials | Apple Health & Ambetter |
| CP.MP.127 | Total Artificial Heart | Apple Health & Ambetter |
| CP.MP.137 | Fecal Incontinence Treatments | Apple Health & Ambetter |
| CP.MP.249 | Omisirge (omidubicel): Nicotinamide-modified allogeneic hematopoietic progenitor cell therapy | Apple Health & Ambetter |
The below Infectious Disease policies were updated as part of our regular monthly review in July. The policy changes are effective November 1, 2024. You will find the policies, including a description of the revisions, posted on the policy site. These policies will be enforced via claim payment edits.
| Policy Number | Policy Title | Line of Business |
|---|---|---|
| CG.CP.MP.01 | ID Respiratory Lab Testing | Apple Health & Ambetter |
| CG.CP.MP.02 | ID Multisystem Lab Testing | Apple Health & Ambetter |
| CG.CP.MP.03 | ID Dermatologic Lab Testing | Apple Health & Ambetter |
| CG.CP.MP.04 | ID Gastroenterologic Lab Testing | Apple Health & Ambetter |
| CG.CP.MP.05 | ID Primary Care Preventive Lab Testing | Apple Health & Ambetter |
| CG.CP.MP.06 | ID Vector-Borne and Tropical Diseases Lab Testing | Apple Health & Ambetter |
| CG.CP.MP.07 | ID Genitourinary Lab Testing | Apple Health & Ambetter |
The below policies were updated as part of our regular monthly review in July. The policy changes are effective December 1, 2024. You will find the policies, including a description of the revisions, posted on the policy site.
| Policy Number | Policy Title | Line of Business |
|---|---|---|
| CP.MP.93 | Bone-anchored hearing aid | Apple Health & Ambetter |
| CP.MP.129 | Fetal Surgery in Utero for Prenatally Diagnosed Malformations | Apple Health & Ambetter |
The below policies were previously announced as revised on the date noted. You will find the policies posted on the policy site.
| Policy Number | Policy Title | Effective Date | Line of Business |
|---|---|---|---|
| CP.MP.40 | Gastric Electrical Stimulation | 9/1/24 | Apple Health & Ambetter |
| CP.MP.91 | Obstetrical Home Health Care Programs | 9/1/24 | Ambetter |
| CP.MP.132 | Heart-Lung Transplant | 9/1/24 | Apple Health & Ambetter |
| CP.MP.141 | Non-Myeloablative Allogenic Stem Cell Transplants | 9/1/24 | Apple Health & Ambetter |
| CP.MP.185 | Skin and Soft Tissue Substitutes for Chronic Wounds | 9/1/24 | Ambetter |
| WA.CP.MP.185 | Skin and Soft Tissue Substitutes for Chronic Wounds | 9/1/24 | Apple Health |
| CP.MP.176 | Outpatient Cardiac Rehabilitation | 10/1/24 | Ambetter |
| CP.BH.201 | Deep TMS for OCD | 10/1/24 | Ambetter |
| CP.MP.69 | Intensity-Modulated Radiotherapy | 11/1/24 | Apple Health & Ambetter |
| CP.MP.107 | Durable Medical Equipment (DME) and Orthotics and Prosthetics Guidelines | 11/1/24 | Apple Health & Ambetter |
| CP.MP.146 | Sclerotherapy and Chemical Endovenous Ablation for Varicose Veins | 11/1/24 | Ambetter |
| WA.CP.MP.522 | Varicose Vein Treatment | 11/1/24 | Apple Health |
| CP.MP.184 | Home Ventilators | 11/1/24 | Apple Health & Ambetter |
______________________________________________________________________________________
Training/Education
Centers of Excellence One Day Training: HCA is excited to forward an invitation for MCO participation in the Autism Center of Excellence (COE) Certification Training. COE Training is open to health care professionals who are pursuing diagnosis certification, and, to non-diagnosing professionals working in the health care industry such as registered nurses, care, or case coordination professionals, claims staff, etc. Please also note that the COE has provided a link to the COE Quick Start Guide here.
Friday, September 13 from 8:30AM to 4:30PM – Registration link.
ASAM Criteria 4th Edition Training: Multiple dates available here (PDF).
IECMH Provider Spotlight recording: HCA is hosting a series of Provider Spotlights, focused on mental health assessments for young children. During the Spotlights, providers share about the steps they took to put infant-early childhood mental health (IECMH) services into practice. At the July Provider Spotlight, providers from Greater Lakes Mental Healthcare and Ryther shared about how they’ve shifted their intake workflows to better support multi-session assessments and use of the DC:0-5. If you missed the session, watch the recording to hear about concrete strategies for topics like scheduling sessions, assigning staff, updating EHRs, and engaging with caregivers.
Want to learn more?
HCA will host additional Provider Spotlights over the next year. These sessions are a great way to connect with and hear from other providers who are learning as they go.
- October 24, 2024: Structuring Assessment Sessions and Cultural Considerations
- January 23, 2025: Screenings, Collateral Information, and Referrals
- April 24, 2025: Assessments in Natural Settings

